Sacroiliac Joint Dysfunction
Stop suffering from sacroiliac joint dysfunction
Thank you for visiting our website. We are glad you have made this important first step towards overcoming your Sacroiliac Joint Dysfunction. Many patients have managed their own sacroiliac pain and health care needs and so we value your time spent with us. We strive to offer you personalized service and provide you with relevant information and treatment options that are best suited to your own unique sacroiliac joint dysfunction.
To ensure you have the greatest opportunity for a full recovery from this debilitating condition, we offer a comprehensive care plan for EVERY step of the way. Our SI joint pain management team will co-ordinate your complete medical care itinerary from beginning to end covering both the conservative treatment and surgical treatment options.
Millions of people suffer with lower back pain. It is a common complaint which may persist for months or years. Much of what is thought of as “lower back pain” is actually caused by a ligament sprain or sacroiliac joint malalignment. Sacroiliac joint pain is one of the most commonly misdiagnosed causes of lower back pain. This is because only a few health care professionals are trained to identify the specific symptoms that indicate a sacroiliac joint problem. Sacroiliac joint dysfunction does not usually show up on X-ray, MRI or CT scans and so this makes it difficult to accurately diagnose.
In order to understand the nature of your injury and what can be done to relieve the pain, a specially trained health care provider such as our experts MUST perform a physical examination to evaluate how the sacroiliac joints are functioning in relation to the rest of the body. We specialize in diagnosing and treating SI joint pain as well as the related disorders such as piriformis syndrome, sacroiliitis and malalignment syndrome. Take the first step towards your recovery and call us today!
Anatomy
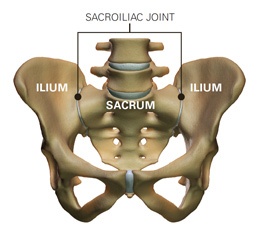
The sacrum is the lower portion of the spine where several vertebrae are fused together. The sacrum is a triangular shaped bone that has a joint on either side with the ilium, the back part of the pelvis. The pubic rami, the front part of the pelvis, fit together in the front forming the pubic symphysis. The sacroiliac joints are L shaped in contour with a shorter upper and longer lower arm. Normally the sacroiliac joint is configured in such a way that the bones have an interlocking structure, which assists in keeping them properly aligned. In some cases the opposing joint surfaces are quite flat. This type of joint is much less stable and can lead to a shearing or sliding malalignment. Some sacroiliac joints reverse the normal concave-convex ‘locking’ relationship, which can lead to rotational malalignment. The variation in joint configuration results in a corresponding variation in integrity. This means that some people are more susceptible to SI joint pain because the joints are inherently weaker or more prone to malalignment.
Causes
There are several different factors that can cause SI joint pain and dysfunction. One of the most common causes is an injury. The injury can come from a direct fall on the buttocks, a motor vehicle accident or a sports related trauma. The force from these injuries can strain the ligaments around the joint. Tearing of these ligaments can lead to hypermobility in the joint. This excess motion and lack of stability is thought to be the main cause behind sacroiliac joint dysfunction.
Pregnancy may also be a factor in the development of SI joint pain. Women secrete the ‘relaxin’ hormone during pregnancy. This hormone allows the connective tissues in the body to relax. The relaxation is needed so the pelvis can stretch enough to allow the baby to pass during labor. This stretching may affect the SI joints causing them to become hypermobile. The more pregnancies a woman has, the more chance she has of developing SI joint pain.
Leg length discrepancies may also play a role in sacroiliac joint dysfunction. If a person has one leg that is shorter than the other, the abnormal alignment may end up causing SI joint pain or malalignment issues.
Often, an exact cause leading to SI joint pain cannot be found. The joint simply becomes painful, and the patient and their local physician do not have an answer as to why the joint has become troublesome. It takes a trained health care provider to accurately diagnose and treat sacroiliac joint pain.
Signs and Symptoms
The most common manifestation of sacroiliac joint dysfunction is acute pain in the low back, in the area of the Posterior Superior Iliac Spine (PSIS) positioned approximately 2 inches from the midline and very deep-seated. Usually, tenderness is found near the lumbo-sacral promontory and in the PSIS area, one more pronounced than the other. Radiating pain into the buttock, hip, groin and thigh is often experienced. The pain is frequently increased by prolonged positions such as sitting, standing, walking or lying. The patient reports that frequent position changes are needed to maintain any degree of comfort.
Common symptoms of sacroiliac joint dysfunction:
- Lumbosacral pain
- Buttock Pain
- Pain radiating to the leg
- Hip pain
- Groin pain
- Urinary frequency
- Iliac crest pain
- Transient numbness, prickling or tingling
- Increased pain with menstruation
- Increased pain with sexual intercourse
- Increased pain with stair climbing
- Increased pain with sustained positions (i.e., sitting, walking, lying)
Patient self-evaluation of symptoms revealed the following:
- 96% Increased discomfort with sustained positions (i.e., standing, sitting, lying)
- 66% Radiating buttock pain
- 39% Discomfort with stair climbing and/or hill climbing
- 26% Groin pain
- 23% Radiating leg pain
- 20% Pain with forward flexion
- 15% Loss of strength in the legs
- 10% Urinary frequency
The most commonly reported position of comfort by patients in the study was side lying (left or right), with a pillow between the knees.
The most frequent complaint from patients with sacroiliac joint dysfunction is increased discomfort with sustained positions such as standing, sitting and lying, with the inability to attain a position of comfort. A disc patient can often find a position of comfort, especially when lying down. Sacroiliac joint symptoms will intensify with activity and decrease with rest, while disc symptoms will usually be worse upon rising in the morning.
The second most common symptom of sacroiliac joint dysfunction is radiating buttock pain. This is reported as a generalized distribution of “achiness” which can radiate into the thigh.
The third most common symptom is increased discomfort with stair or hill climbing. This is a result of increased demands on the skeletal and soft tissue system of the pelvic girdle during these activities. This symptom may also be present in disc pathologies, but is primarily reported as increased discomfort with forward trunk flexion.
Diagnosis
A clear understanding of the difference in the signs and symptoms of sacroiliac joint dysfunction and other pathologies is key in making the proper diagnosis. The diagnosis of sacroiliac joint dysfunction is made primarily from the patient’s subjective complaints and the physical evaluation; therefore, a diagnosis can be somewhat problematic for the clinician. Sacroiliac joint dysfunction does not usually show up on X-rays, MRI, or CT scans and so this makes it difficult to accurately diagnose. The most accurate way of determining whether the SI joint is a pain generator is to perform a diagnostic injection directly into the joint. Because the joint is so deep, this must be done using X-ray guidance with a fluoroscope. A numbing agent and steroid is injected directly into the joint. If the patient reports a drastic improvement in pain, then the physician may conclude that the SI joint is a pain generator.
Associated Conditions
Sacroiliac joint dysfunction can occur as an isolated condition, or associated with other spinal disorders. Torsion injuries can cause damage to the disc annulus, facet joints, lamina, pedicle and ligaments, as well as to the sacroiliac joint.
Common associated conditions of sacroiliac joint dysfunction:
Facet Joint
Torsion or axial rotation causes the facets to flex and laterally bend towards the side of the rotation crushing the facet articular surfaces on the rotation side and distracting the capsule with tearing or avulsion on the side opposite the rotation.
Nerve Root
The lateral portion of the facet joint is long and slender, making it easily deformed. Torsion causes facet impingement on the torsion side. Distraction on the opposite side can stretch the nerve root. Therefore, neural arch deformation can cause bilateral nerve root entrapment.
Disc
Torsion causes annular tears which can weaken the annulus leading to an annular bulge, or herniation, of the nucleolus pulposis. The iliolumbar ligament can become taut due to sub-luxation of the sacroiliac joint. Its fibers are attached to the transverse process of L4, and chronic tension can lead to bulging of the disc. It is not uncommon to see an L4 annular bulge on the MRI of a patient who has chronic sacroiliac joint instability.
Effect on muscle and piriformis syndrome
Janda, an expert on muscle imbalance, has pointed out that postural muscles become facilitated and tighter, and phasic muscles become inhibited and weaker as the result of articular dysfunction. With long-standing dysfunction, anatomic changes in the muscle bundles can take place that are irreversible. Ther piriformis is one of the most adversely affected muscle in chronic sacroiliac instability (piriformis syndrome). Pelvic wall muscle spasm, or contracture, may lead to pelvic floor dysfunction. Other muscles affected include the iliopsoas, hamstrings, adductors, gluteus, quadratus lamborum, and the tensor facscia lata.
Effect on nerves
Due to long-standing spasm, or secondary fibrosis, the chronically shortened piriformis can entrap neurovascular structures that accompany it through the greater sciatic foramen (superior and inferior gluteal nerves, the sciatic nerve and the pudendal nerve. The lateral femoral cutaneous nerve passes just medial to the anterior superior iliac spine. It can be injured as it passes form the pelvis to the thigh by changes in anatomic positioning associated with sacroiliac joint subluxation (meralgia paresthetica).
Pubic symphysis instability
With chronic sacroiliac joint instability the contralateral sacroiliac joint and the pubic symphysis may destabilize.
Conservative Treatment
Initial treatment is provided by a physical therapist skilled in diagnosing and treating sacroiliac joint pain. Following evaluation and mobilization treatment the therapist will instruct the patient on proper biomechanics to avoid unnecessary and improper strain on the injured si joints. Therapeutic exercise is taught to improve neuromuscular stability of the lower back and pelvis. Self-mobilization techniques are instructed to the patient. Too much movement of the sacroiliac joints may indicate a laxity of ligaments that would normally hold these joints within a normal range of motion. Therefore, additional stabilization procedures, for example pelvic belt fixation and taping techniques may be required. A home program of self-mobilization is necessary: either by self-mobilization exercise or by family members who have been taught to do the family assisted corrections.
Typically the sacroiliac joint dysfunction will stabilize with a good stabilization program over a 6-8 week period of time. Medical options such as prolotherapy, platelet-rich plasma injections (PRP) or surgery may be indicated for those patients who continue to demonstrate too much mobility in the SI Joint after rehabilitation. Our clinicians recommend a series of 6 prolotherapy or platlet-rich plasma sessions spaced between 14-30 days if you continue to experience SI Joint instability after a 6 week trial of Physical Therapy by a skilled expert. Prior to your injection it is recommended that your SI joint be mobilized into proper alignment and maintained with self-correcting and family assisted techniques to allow for adequate tissue healing. Taping and belting are also highly recommended during the 2-3 month period you are receiving the injections.
Gainesville Physical Therapy specializes in the evaluation and treatment of sacroiliac joint dysfunction. Our therapists are the leaders in this field and therefore see patients from all over the United States, Canada and the rest of the world. Most patients receive all of their treatment in our offices, while some are evaluated and referred back to local experienced physical therapists with a recommended treatment plan.
Surgery
For more information on our surgical treatment options click here