M.D. Avillar J. G. Keating V. Sims
_______________________________________________________________________________________________________
lNTRODUCTION
Incidences of lower back pain continue to escalate, both in number and in total cost to health-care systems (Kelsey & White 1980). This trend of increased injury and cost continues in spite of large increases in research and funding that is directed at all areas of spine care. Low back pain is a 50 billion dollar a year growth industry in our society (Graves et al 1990a).
Waddell (1980) nates that there has been an epidemic of low back pain in the Western world since 1956. The reason behind this phenomenon is unclear; however, it is believed that the increase can be attributed to increasingly sedentary lifestyles and the sedentary work roles that are developed in a society based on information.
Treatment plans that deal with chronic low back pain have not changed in their basic make-up for the past 40 years. The most common method of treatment for any form of low back pain is bedrest and analgesics. However, there is no documentation that this is an effective treatment regime (Twomey & Taylor 1995).
Exercise has been proposed to remedy low bade pain since Samuel Gowers (1904) advocated an active rehabilitation program for his patients. Exercise as a form of treatment is only now gaining widespread acceptance as an effective method of dealing with low back pain. A number of differing types of exercise have been prescribed to deal with chronic low back pain. The different forms of exercise training vary widely from the rarely used heavy resistance training, general conditioning, cardiovascular endurance training, and training with light weights at high repetitions, to any number of various combinations (Foster & Fulton 1991). Clinical settings have generally utilized a basic general conditioning approach teamed with lower body stretches, Williams flexion stretches, McKenzie extension stretches, and physical therapy modalities (Polatin 1990).
Increasing the strength of the low back muscu-lature has been postulated to prevent low back pain (Foster & Fulton 1991, Graves et al 1990a, Kelsey & White 1980, Waddell 1980). The specifics of how actually to increase the strength of the lower back is an issue of debate among clinicians (Rissanen et al 1995). Resistance exercises that are effective in strengthening extensors of the low back region are hotly debated (Pollock et al 1989). The erector spinae that dominate the low back region present a unique problem of how to isolate the muscle group for strengthening. In common everyday activity, the hip flexors and gluteals overpower the lumbar extensors and shield them from exercise (Graves et al 1994). The shielded lumbar extensors may predispose the low back to injury and the development of a chronic pain cycle. Machine-driven lumbar rehabilitation designed to isolate the lumbar extensors has begun to show strong results in decreasing subjective patient pain reports and restoring subject functional status (Carpenter et a1 1991, Nelson et al 1995, Risch et al 1992).
An area relevant for low back pain that has attracted increased scrutiny in the past 10 years is the sacroiliac joint (SIJ). This new-found interest in the SIJ deals with the possible relationship that the SIJ has with chronic low back pain. The SIJ as an area of pain generation has been overlooked since Mixter and Barr introduced the herniated nucleus pulposus (HNP) to the medical world (Mixter & Barr 1934). Prior to Mixter and Barr’s
HNP observations, the SIJ was frequently cited as a possible etiology for pain in the low back (Vleeming et al 1993). Fifty years after the initial realization that the lumbar disc is involved in low back pain, the idea of the herniated lumbar disc mediating all forms of low back pain syndromes has been discounted. It seems quite obvious that there are a variety of structures associated with low back pain; these can be commonly damaged in vigorous or in repetitive daily activities.
A number of problems arise in dealing with the accurate diagnosis of SIJ dysfunction SIJD). One problem occurs in that the pain patterns are similar to those of other common low back pain disorders. A diagnostic conundrum presents owing to the fact there are no concrete uniform criteria dealing with SIJD (van Duersen et al 1990). Practitioners have in the past dumped a number of indiscernible low back pain problems into the SIJD category. This practice has led, historically, to a lack of credibility being given to the diagnosis of SIJD. Another problem involved with the diagnosis of SIJD is the nature of the activity that causes the injury. Activities that can commonly cause SIJD (Box 41.1) are very similar to activities that are found to cause more commonly accepted low back pain disorders. Owing to these diagnostic and historical problems, a common practice of overlooking SIJD as a possible pain source has evolved in most mainstream orthopedic practices (Shaw 1993). In most circles, the diagnosis is completely overlooked or cast off as one of quackery.
Theories relating to a possible pain mechanism associated with SIJD come from a number of areas: muscle imbalance, regionalized muscle or ligamentous sprain/strain, sacral and/or ilial mis-alignment and SIJ capsule tears. Sacroiliitis is considered to be the most common form of SIJ pain (Bernard & Cassidy 1993). The exact mechanism causing the inflammation at or near the SIJ is frequently unclear. Muscle imbalance has also been cited as a possible cause of pain. The muscle imbalance theory maintains that the joint itself is unaffected, but that the musculature surrounding the SIJ is in some form of dysfunction (Kermond 1995). This dysfunction could limit the flexibility of the dynamic muscles of the low back and ultimately begin a syndrome of chronic disuse, culminating in decreased function and pain. SIJ capsule tearing could occur from an intense trauma to the SIJ or from a shearing type movement and/or blow to the SIJ. This over all degeneration of the connective sheath surrounding the SIJ has provoked growing interest in radiologists and orthopedic surgeons. SIJ capsule ruptures are observed by injecting into the joint capsule contrast materials that can provide radiographic evidence of abnormality (Schwarzer et al 1994).
The treatment protocol described in this article utilizes an extensive evaluation of the SIJ. If SIJD is diagnosed, a manual correction technique is employed; this technique is aimed at producing symmetric bony landmark alignment for the SIJ and the surrounding structures. Arfter the manual therapy is completed, an aggressive specific lumbar extensor resistance exercise program is undertaken. The evaluation of program success involves the change in subjective complaints of pain, objective changes in subjective lumbar extensor strength and objective change in subject work status prior to and following the protocol. This project is part of a resurgence among conventional mainstream caregivers (medical doctors, orthopedic surgeons, exercise therapists and physical therapists) who have become interested in SIJD as a possible cause for chronic low back pain.
METHODS
Worker’s compensation subjects presented to an orthopedic surgeon’s practice because of low back pain. The low back pain had to be of a chronic nature (4 weeks or longer) to be considered for this project. All subjects presented with specific complaints of pain in the SIJ area. The specific low back pain complaints were documented by use of pain diagrams (Schwarzer et al 1994). Subjects were examined for low back pain and showed no neurological signs of lumbar disc abnormality.
The diagnosis of SIJ dysfunction was determined by the anatomic location of patient pain, response to SIJ provocation testing and manual testing abnormalities seen during movements that are combined with bilateral symmetry abnormalities. If one or more of the tests in each category was positive, and a specific region of pain was present at the SIJ, the patient was diagnosed as having SIJD. The series of tests that are used to diagnose SIJD are seen in Boxes 41.2-41.4.
Manual dynamic testing
The supine long sitting test is performed with patient supine on an examining table. The examiner begins by placing his thumbs under the inferior border of each medial malleolus. The two medial malleoli are brought together for comparison, the knees being fully extended and all musculature relaxed. The patient then flexes into the seated position with knees extended, while looking at the ceiling. Again, the lower body musculature should be relaxed. Great care is taken to make sure the subject is in a symmetric position ar all times; if not, a false positive can occur due to patient positioning. The test is positive if the positioning of the malleoli, comparing pre-long sit and post-long sit, has created a discrepancy. The discrepancies between the malleoli during the long sit test are assessed for non-symmetric interaction. A positive test results when observable change occurred in relative leg length differences between the two positions.
The standing flexion test is performed with patient standing, knees straight, and feet pointing straight ahead. The examiner’s thumbs are placed on the inferior aspect of the left and the right posterior superior iliac spine (PSIS). The patient bends slowly forward as far as possible. A positive test occurs when one PSIS has moved more cranially than the opposite PSIS.
The sitting flexion test is performed when the patient is in a seated position on the table. The examiner’s thumbs are placed on PSISs, and the patient is then asked to bend forward slowly from the neutral position. The gluteals should not be allowed to lift off the examining table. A positive test occurs if one PSIS moves to a superior position with respect to the other. The superior PSIS is considered to be the dysfunctional side. The standing flexion test is the same design as the sitting flexion test except that the subject is standing and may not bend his knees.
The march/stork test is performed as the patient is standing in the neutral position. One of the examiner’s thumbs is placed on the right PSIS while the other thumb is placed on the dorsal surface of the sacrum, placing the thumbs into a position of alignment. The patient then flexes at rhe hip on the side being examined. The PSIS should travel in a downward direction in comparison to the thumb acting as sacral marker. If there is no downward motion of the PSIS that is being examined, the test is considered to be positive.
Static symmetry tests
Assessment of bilateral ASIS symmetry occurs with the subject in the supine position. Anterior superior iliac spine (ASIS) positioning is carried out by placing the volar surface of the distal thumb on the underside of each ASIS. The height of each spine is compared in a horizontal plane. A positive ASIS test results when the height of one of the ASIS’s is greater than that of the opposite ASIS.
Assessment of the iliac crests occurs as follows. The apexes of the iliac crests are found with the subject in the supine position. Iliac crest positioning is carried out by placing the volar surface of the proximal index finger on the crest of the ilia. The height of each ilium is compared, utilizing the finger positioning, in a vertical plane. Great care should be taken to ensure that the subject is in a symmetric position when being assessed. A positive iliac crest test results when the height of one of the iliac crests is superior to that of the opposite one.
Assessment of bilateral PSIS symmetry occurs with the subject in the prone position. PSIS positioning is done by placing the volar surface of the distal thumb on the dorsal surface of each PSIS. The height of each PSIS is compared with that of the other in a horizontal plane. A positive PSIS test results when the height of one of the PSIS’s is greater than that of the opposite one. This test is difficult to assess when subjects are obese.
Assessment of sacral obliquity occurs with the subject in the prone position. The dorsal surface of the coccyx is bilaterally palpated using the volar surface of the distal thumbs. In this part of the assessment, the thumb should act as an outliner and not as a pressure point on the landmarks (pressure in this test can be used to detect whether the sacrum is tender to touch at the sacral borders and the PSIS). The examiner should move his thumbs cranially up the sacral border to each fused segment of the sacrum.
At each fused segment of the sacrum the heights of the bony landmarks should be compared with each other in the horizontal plane. If one thumb is more posterior than the other, a positive test has occurred. It is a common occurrence in SIJD to elicit pain with pressure at different sacral segment levels. This production of pain can be used as a diagnostic tool for SIJD. The pubic symphysis is located on the subject in the supine position. Both thumbs are placed on the anterior portion of the pubis. If one thumb is more posterior than the other, the test is positive. Another sign that the pubic symphysis is mediating pain is a sharp pain in the groin when the manual correction technique is being performed. This is most notable during the setting of the pubes (see below).
Diagnostic Assessment
The assessment procedure for SIJD takes into account a number of signs and symptoms. In order to diagnose SIJD, the evaluator should have a combination of results: positive pain pattern for SIJD (Fortin et al 1994a, 1994b), an objective result in SIJ testing, and abnormal static SIJ landmarks (Shaw 1993). Pain generation upon provocation testing is a positive indicator of SIJD, as is having a common SIJD injury mechanism in the history. The SIJD provocative testing and common injury mechanisms are not, however, an absolute necessity for making the diagnosis. The different SIJD tests and signs are described in Boxes 41.2-41.4 (descriptions of the static and dynamic tests are given in the previous section). If there is no pain over the SIJ region, or pain cannot be alleviated by manual mobilization, the subject should not be considered to have SIJD. No particular set of diagnostic criteria is generally used for the diagnosis of SIJD. The lack of a “gold standard” in the diagnosis of SIJD is in part due to great differences in the literature about which SIJ test can be used as a valid predictor of SIJD (Cibulka et al 1993, Laslett & Williams 1994, Potter & Rothstein 1985). Patients who are acutely injured (4 weeks or less) are not suitable for discussion of this SIJ treatment protocol. The majority of low back pain cases will naturally resolve in a 4-6 week period (Andersson 1981).
It should be noted that if the only objective measure for low back pain is asymmetric align-ment of the ilial and sacral landmarks, this asymmetry alone is not enough evidence for the diagnosis of SIJD. Landmarks that are asymmetric are very common in asymptomatic subjects, as well as in low back pain sufferers and subjects with SIJD. Visualized abnormality on static or dynamic testing can be expected in asymptomatic patients, and painless SIJ asymmetry may not mediate low back pain. If the proper symptoms and pain patterns are not present, other diagnoses should be explored. The overzealous application of these SIJ correction techniques can only water down the overall understanding of the effectiveness of manual correction in a chronic low back pain population.
The series of steps behind the overall diagnosis for SIJD is as follows: low back pain assessment utilizing extension, flexion, or lateral side-bending movements to alleviate pain and/or numbness in lower limbs or low back (Donelson 1980). If these treatment measures do not resolve the situation, the subject’s history should be checked to see whether SIJD is indicated. It should be elicited that pain patterns are physiologic for SIJ injury (Fortin et al 1994a, Waddell 1980, Keating et al 1995). Patient ilial and sacral landmarks (Box 41.4) should be evaluated for possible asymmetry, and SIJ dynamic and provocation testing (see Boxes 41.2 and 41.3 above) conducted. Manual correction techniques are utilized to produce symmetry in pertinent landmarks (see below). It should be observed whether manual corrections increase the pain-free end of range flexion/extension movements and/or decrease subjective pain ratings in the low back.
Treatment
The rehabilitation process consisted of the symmetric alignment of the SIJ’s bony landmarks utilizing manual mobilizations. Following the manual corrections, an extensive dynamic resistance training program (MedX, Ocala, FL, USA) specific to the lower back was performed, in conjunction with the introduction of a general conditioning program. The general conditioning program consists of machine progressive resistance exercises (PREs) for the legs, upper torso and abdominal muscle groups. In addition, a common program of lower body and lumbar extension stretching was given for home use.
On the first visit to the rehabilitation area, the subjects were manually mobilized into symmetric sacral and ilial positions and given a home exercise program that had basic pelvic stabilization and flexibility stretches, and McKenzie extension exercises. On the second visit to the rehabilitation unit, the SIJ was re-evaluated. Following the manual correction, the patient was then assessed for initial isolated lumbar strength. The assessment of patient back strength was determined by the utilization of an isometric strength testing device. The testing device used was a MedX lumbar extension unit as described by Avillar (1995) (see also Chapter 46 in this volume).
After the, initial strength test (visit 2), the subjects began dynamic training on the lumbar extension machine. The dynamic training consisted of a concentric and an eccentric movement phase, the eccentric phase being emphasized. The training was performed until the subject reached volitional muscle failure, i.e., he lifted the weight until he could no longer exercise. The goal of this training is an exercise session of l set, 12-20 repetitions, in a 75-120 s period. The volitional failure method (Pollock et al 1989) utilizes a progressively heavier weight at exercise, the weight being slowly lifted each time until it cannot be lifted correctly (no preset number of repetitions). If 15-20 repetitions were successfully completed in 110+ s, the training weight for the next session would be raised by 10%. The training regimen continued twice per week until the patient was discharged. Isometric tests were administered once a month.
Manual mobilization of SIJD
The sacroiliac (SI) manual corrections that were performed on the SIJD population were always in the order of correcting iliac non-symmetry, then ASIS discrepancy, and finally sacral obliquity. Iliac positioning was considered to be of greater importance than possible non-symmetric sacral positioning. Hence, iliac asymmetry was treated before any sacral rotation. It is important to note that many different iliac and sacral alignment procedures have appeared in the literature (e.g. Cibulka 1993, Keating et al 1995).
The following methods were used for manual mobilization, these being selected because of the therapists’ familiarity with the systematic pro-cedure. This familiarity had been developed by over 10 years of experimentation with different SI mobilization techniques.
After the diagnosis of SIJ involvement is made, the following manual corrections should be performed. If a subject presents with one ilium superior to the other, the term “upslip” is applied to the superior side. This iliac upslip in the supine position (observed with the long sit, iliac crest, and ASIS tests; see Box 41.3 above) is treated with the subject supine, the leg on the superior side being externally rotated and fully extended. The leg is then held in a fully extended, relaxed position at 30-45° from the table. A gentle but forceful sustained traction is applied to the leg in a series of three pulling motions. If the traction maneuver does not produce symmetric ilial positioning, reproduce the mobilization. If the subject presents with an iliac upslip in the prone position (observed with the long sit, PSIS, and iliac crest tests; Box 41.4), treatment follows the aforementioned steps for an upslip, but the subject is in the prone position. The traction force should not cause any pain to the subject.
If the right ilium is rotated into a posterior position, the right ASIS will be depressed and/or more cranial than the left ASIS. If the ASIS’s are not in symmetric positions, the following corrections (the “push-pull” technique) are used. The technique activates the hip flexors on the right and the hip extensors on the left. As the subject is supine with the hips flexed at 90° and the knees bent, the examiner has the subject pull the right knee toward the chest while the examiner provides resistance above the knee in the anterior thigh. The left knee is simultaneously driven in a downward direction in which the examiner also resists the movement in the posterior thigh. These movements are isometric contractions performed 3-5 times per session, with a resistance applied for 3-5 s. The patient movement force is at an exertion level of 80-100%. If the left ilium is rotated into a posterior position, the aforementioned corrections are used with the actions of the hip extensors and hip flexors being reversed.
If the right ilium is rotated in an anterior position, the right ASIS will be elevated and/or posterior to the left ASIS. The aforementioned “push-pull” method will be used again, this time activating the hips extensors on the right and hip flexors on the left. If the left ilium is rotated in an anterior position, the same mobilization is used in accordance with the right ilium anterior rotation technique, the only difference being the use of the opposite limbs from those in the description above.
If the sacrum is rotated in a posterior position on the right side, the following technique is used for correction. The subject lies on his right side with the hips flexed at an angle of approximately 70-80° (almost a fetal position). The right knee is flexed at a 90° angle, and the left leg is fully extended and relaxed over the right thigh. The examiner places one hand under the subject’s right knee and the other hand on the medial side of the right ankle. The subject holds the right leg up at approximately 30-50° while the examiner pushes the leg down using the hand positioned on the ankle (dynamic contraction). This movement is repeated in a series 3-5 times.
If SIJD is present, and the mobilization is done correctly, the patient will feel a pulling sensation in both the PSIS’s. The more notable sensation is in the opposite PSIS when the subject is lying on one side. It is of great importance that the quadriceps and/or the hamstrings are not activated when this “piriformis” exercise is performed. If these muscles are active in the contraction, the resistance to the examiner’s movement will be much greater and the pressure to the movement will be felt in the patient’s quadriceps or hamstrings instead of the PSIS’s.
If the sacrum is rotated posteriorly on the left side, the same technique is used as described above for the right rotated sacrum. The only differences are that the subject will lie on his left side and the movements are carried out on the left leg.
If the right symphysis pubis is superior to the opposite pubis, the following mobilization will produce symmetry and decrease pain when adducting the knees at the end of the mobili-zations (setting the pubes). The subject will activate the left rectus abdominis and the right hip adductors. While the subject is supine, he is instructed to push his left shoulder off the table (in a sit-up style contraction) while the examiner provides resistance to the movement at the shoulder. When the subject’s torso has lifted 5-10 cm off of the table, the movement is blocked by the examiner. The right hip is flexed at 45-55° and will simultaneously adduct, the examiner providing resistance to the movement above the knee. These movements last 3-5 s and are performed in a series of three.
The same mobilization as described in the paragraph above is performed if the left symphysis pubis is superior to the right and if a sharp pain is present in the groins when setting the pubes. The only difference is that the opposite movements are conducted for a left, as opposed to a right-sided problem.
After all of the necessary manual mobilizations have been completed, and symmetric alignment has been achieved, mobilization of the pubes will be last (this is referred to as setting the pubes or “shot-gunning” the pubes). In this technique, the subject is supine with the hips flexed at 45° and the feet positioned almost side by side (in a “butterfly position”). The examiner’s elbow is placed at one side of the inner knee, the other hand locking down on the opposite inner knee. The subject is instructed to adduct his knees together at 80-100% of maximal force for 3-5 s. This is done three times. It is common for an audible click to be present, which should not be painful. After setting the pubes, the sacral and ilial landmarks are checked for symmetry, objective dynamic testing is performed, and the subject can describe pain changes.
The observation of the bony landmarks and the dynamic tests will not always go to a perfect degree of symmetry. If the asymmetric bony landmarks occur after mobilization, and pain has not been alleviated, the SIJD subject should be re-evaluated and the maneuvers performed again. If symmetry is never gained, it may not be a plausible goal. This may be due to intrinsic asymmetric landmarks, lack of clinician expertise, or lack of pain generation from the SIJD complex. It has been this team’s observation that these cases are in a large minority of SIJD sufferers.
Pain scores. Subjects were asked to score their pain level prior to each rehabilitation session. The pain rating was the average level of pain that the subject felt before entering the building for rehabilitation. The visual analog scale for pain rating that was used is as follows:
0 No pain
1-2 Occasional pain
3-4 Mild constant pain
5-6 Moderate constant pain
7-8 Unable to carry out daily activities
9-10 Emergency: need to see a doctor.
Work status. Subject work status was taken at the initial visit and on discharge from the program. The following rating system accompanied the subject’s level ofwork:
0 No work
1 Sedentary duty
2 Light duty
3 Moderate duty
4 Full duty
Sedentary duty consisted of lifting a maximum 5 kg and occasionally lifting and carrying such articles as dockets, ledgers, and small tools. Light duty consisted of lifting a maximum of 10 kg. with frequent lifting and/or carrying of objects weighing up to 5 kg. Moderate duty consisted of lifting up to 25 kg and frequent lifting and/or carrying of objects weighing up to 10 kg. Full duty consisted of the normal 40 hour-a-week job that was done prior to injury.
Discharge from the program. Subjects were given a 1-month prescription for (twice a week) physical therapy. At the 1 month mark, subjects were reviewed for the following criteria: strength improvement, compliance to program, and pain status. Criteria for discharge from the program included: goals being achieved, non-physiologic strength decreases at isometric (IM) testing, and continued non-physiologic pain patterns or complaints (Waddell 1980). Consideration of surgery for the SIJ occurred if patients went through the rehabilitation program, did not receive relief after 8 weeks of treatment, and continued to report physiologic pain patterns (Schwarzer et al 1994).
RESULTS
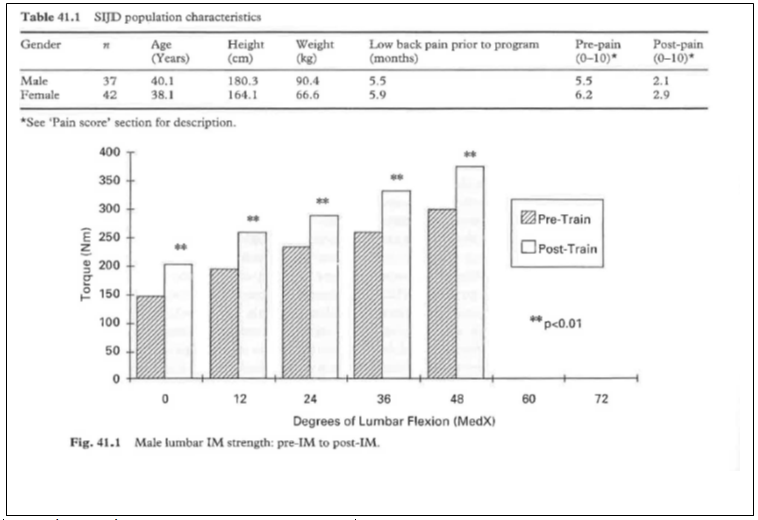
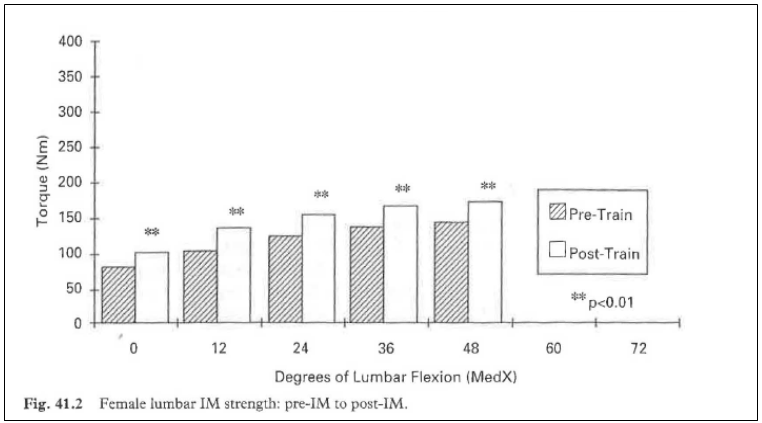
Forty-two females qualified for SIJ mobilization and isolated lumbar strength analysis in a 6-month period from March to September 1994. For gender population characteristics, see Table 41.1. Analysis of variance (ANOVA) reveals that the average pain score on the visual analog scale significantly decreased (p < 0.001), from an initial 6.2 to final average of 2.9. ANOVA reveals that work status increased significantly (p < 0.001) from an initial average work level of 2.6 to a discharge work level of 3.7. The average IM torque increased significantly (p < 0.01) from an initial IM average of 123.9 IM to a final IM average of 153.5 Nm (+23.8%). ANOVA showed that IM torque increased significantly (p < 0.01) at all standardized test points throughout the pain-free range of motion (ROM) during IM testing (Fig. 41.1). The pain-free ROM did not change during the program. The average number of rehabilitation visits for the female population was 15.4 sessions.
Thirty-seven males qualified for this analysis from March to September 1994. ANOVA revealed the following results. The average pain score on the visual analog scale significantly (p < 0.001) decreased from an initial visit average of 5.5 to a discharge average of 2.1 (scale above). Work status increased significantly (p < 0.001) from an initial visit work level of 3.2 to a work level of 3.7 on discharge from the program. The average IM torque scores increased significantly (p < 0. 01) from an initial IM average of 217.1 Nm to a final IM average of 276.1 Nm (+27.2%). IM torque increased significantly (p < 0.01) at all standardized test points throughout the pain-free ROM during IM testing (Fig. 41.2). The pain-free ROM increased significantly (p < 0.01) from initial ROM (0-46°) to final ROM (0-50°). The average number of male rehabilitation visits was 14.3 sessions.
In comparing male and female populations, ANOVA reveals no significant difference (p > 0.05) in initial pain rating, final pain rating, final work status level, length of low back pain previous to SIJ protocol entry, average lumbar
Strength change number of rehabilitation sessions and group age. Significant differences (p < 0.05) occur in total IM torque produced group height, and group weight, the male group having greater values for these three aspects.
DISCUSSION
These data indicate that the SIJ mobilization and isolated lumbar strengthening protocol is effective in reducing subject self-reported pain levels and increasing the subject functional working status. Objective measurements of improvement are witnessed by the increasing strength values seen on lumbar extension strength testing (lumbar IM torque) and in the increasing levels of subject work status. These objective changes occur with subjective decreases in self-reported pain levels in a chronic workers’ compensation low back pain population.
Comparing the male and female group charac-teristics, ANOVA reveals that the populations are homogenous in nature, barring gender-based differences. The areas in which there are no significant differences are numerous. The gender-based differences occur in group height, weight, and the overall total lumbar IM torque produced, differences that are to be expected when comparing male and female groups.
The study of the effects of manual mobilization on the SIJ and low back pain, in general, has yet to be examined. The effects of machine-driven isolated lumbar resistance training on low back pain sufferers, let alone those people who may suffer with SIJD, have yet to be fully investigated. To our knowledge, this is the only study that has had a well-defined SIJD group that was manually mobilized into symmetric SIJ position and then trained in an isolated lumbar extension device. This is also one of the few studies dealing with the SIJ that has objective evidence (increased strength gain, increased work status level) along with subjective reports of decreased pain when utilizing a specific treatment protocol.
This information shows an objective functional restoration of subject strength and work status in a chronic low back pain population within a workers’ compensation population. This protocol warrants scrutiny due to: overall effectiveness, method of SIJD assessment and diagnosis, and the combination of manual treatment and aggressive isolated lumbar machine-driven exercise.
CONCLUSIONS
1. This study reveals very positive results in the areas of self-reported subjective decrease in low back pain, as well as objective increases in lumbar strength and increased functional status (work level).
2. This unique combination of manual therapy and aggressive resistance training in a chronic
low back pain population requires further enthusiastic investigation due to its effectiveness and the efficient treatment period for a traditionally difficult population.
3. An obvious question arises of what the individual effects of the isolated strength training versus the effects of the SIJ mobilization techniques were.
4. The issues behind the causative nature of these results require that this project be investigated at greater length.
5. Two main points involving this population bear mentioning: subjects were utilizing the worker’s compensation system, and they had chronic complaints of low back pain lasting for longer than 5 months prior to entry into this program.
Considering these two important issues in dealing with this study population, the results are remarkable. This evaluation and treatment method for the SIJD is an attempt to treat a subcategory of low back pain that has not in the past been well defined or treated in a consistent manner.
ACKNOWLEDGMENTS
I would like to thank the entire staff at the Keating Group for their help in assembling this chapter. I especially want to thank the amazing interns (Jennifer, Chris Chrissy, Mark and Molly) from the University of Florida who spent countless hours at bizarre and tedious tasks to prepare this information.
REFERENCES
Andersson G 1981 Epidemiological aspects of low back
pain in industry. Spine 6: 53-60
Avillar M, Sims V, Keating J, Stinchcomb P, Herrberg J
1995 The effect of a seven week sacroiliac joint
mobilization and stabilization program on a low back
pain population. In: Vleeming A, Mooney V, Donnan T,
Snijders C (eds) Second interdisciplinary world congress
on low back pam. San Diego, CA, 9-11 November,
pp 305-321
Bernard T, Cassidy D 1993 The sacroiliac joint syndrome:
pathophysiology, diagnosis, and management. In:
Vleeming A, Mooney V, Snijders C, Dorman T (eds)
First interdisciplinary world congress on low back pain
and its relation to the sacroiliac joint. San Diego, CA, 5-6
November, pp 120-143
Carpenter D M, Graves J E, Pollock M et al l991 Effect of
12 and 20 weeks of resistance training on lumbar
extension torque production. Physical Therapy 71: 580-
588
Cibulka M, Delitto A, Erhard R E 1993 Pain patterns in
patients with and without sacroiliac joint dysfunction. In:
V1eeming A, Mooney V, Snijders C, Dorman T (eds)
First interdisciplinary world congress on low back pain
and its relation to the sacroiliac joint. San Diego, CA,
5-6 November, pp 363-370
Donelson R 1980 The McKenzie Approach to evaluating
and treating low back pain. Orthopaedic Review 19(8):
681-686
Fortin A, Dwyer S, West J, Pier J 1994a Sacroiliac joint: pain
referral maps upon applying a new injection/arthrography
technique. I: Asymptomatic volunteers. Spine 19(13):
1475-1482
Fortin A, Aprill C, Ponthieux B, Pier J 1994b Sacroiliac
joint: pain referral maps upon applying a new
injection/arthrography technique. 2: Clinical evaluation.
Spine 19(13): 1483-1489
Foster D, Fulton M 1991 Back pain and the exercise
prescription. Clinics in Sports Medicine 10(1): 197-209
Gowers 1904 Lumbago: its lessons and analogues. British
Medical Joumal I: 117-121
Graves J E, Pollock M L, Carpenter D M et al 1990
Quantitative assessment of full range-of-motion isometric
lumbar extension strength. Spine 15(4): 289-294
Graves J, Webb D, Pollock M et al 1994 Pelvic
stabilization during resistance training: its effect on the
development of lumbar extension strength. Archives of
Physical Medical Rehabilitation 75: 210-215
Keating J G, Sims V, Avillar M D 1995 Sacroiliac joint
fusion in a chronic low back pain population. In:
Vleeming A, Mooney V, Dorman T, Snijders C (eds)
Second interdisciplinary world congress on low back
pain. San Diego, CA, 9-11 November, pp 361-365
Kelsey J L, White A A 1980 Epidemiology and impact of
Low back pain. Spine 5(2): 133-140
Kermond W 1995 Early intervention low intensity exercise
therapy in work related acute lumbar sprain injuries.
Presented at Exercise rehabiliration of the spine: update
’95, Orlando, FL, 6-8 April
Laslett M, Williams M 1994 The reliability of selected pain
provocation tests for sacroiliac joint pathology. Spine
19(1); 1243-1249
Mixter W J, Barr J S 1934 Rupture of the intervertebral
disc with involvement of the spinal canal. New England
Journal of Medicine 211:210-215
Nelson B, O’Reilly E, Miller M, Hogan M, Wegner J, Kelly
C 1995 The clinical effects of intensive, specific exercise
on chronic low back pain: a controlled study of 895
consecutive patients with 1-year follow-up. Orthopedics
18(10): 971-981
Polatin P 1990 The functional restoration approach to
chronic low back pain. Journal of Musculoskeletal
Medicine 7(1): 17-30
Pollock M, Leggett S, Graves J, Jones A, Fulton M,
Cirulli J 1989 Effect of resistance training on lumbar
extension strength. American journal of Sports Medicine
17(5): 624-629
Potter N, Rothstein J 1985 Interrester reliability for selected
clinical tests of the sacroiliac joint. Physical Therapy 65:
1671-1675
Risch S, Norvell N, Pollock M et al 1992 Lumbar
strengthening in chronic low back pain patients. Spine
18(2): 232-238
Rissanen A, Kalimo H, Alaranta H 1995 Effect of intensive
training on the isokinetic strength and structure of lumbar
muscles in patients with chronic low back pain. Spine 20:
333-340
Schwarzer A, Aprill C, Bogduk N 1994 The sacroiliac joint
in chronic low back pain. Spine 20(1): 31-37
Shaw J L J 993 The role of the sacroiliac joint as a cause of
low back pain and dysfunction. In: Vleeming A,
Mooney V, Snijders C, DormanT (eds) First
interdisciplinary world congress on low back pain and
its relation to the sacroiliac joint. San Diego, CA, 5-6
November, pp 67-80
Twomey L, Taylor J 1995 Exercise and spinal
manipulation in the treatment of low back pain.
Spine 20(5): 615-619
Van Deursen L, Patijn J, Ockhuysen A, Vortman B 1990
The value of some clinical tests of the sacroiliac joint.
Journal of Manual Medicine 5: 96-99
Vleeming A, Stoeckart R, Snijders 1993 A short history of
sacroiliac research. In: Vleeming A Mooney V,
Snijders C J, Dorman T (eds) First interdisciplinary world
congress on low back pain and its relation to the
sacroiliac joint San Diego, CA, 5-6 November, pp 5-1l Waddell G 1980 Nonorganic physical signs in low back
pain. Spine 5(2): 117-125